Prostatitis is the most common urological pathology in reproductive men. According to the selection, each third of them at least in their lives experience symptoms that can be interpreted as inflammation of the prostate gland. Although there is a high pathology, prostatitis remains a less learned disease.To this day, there is no consensus that it is the beginning factor in inflammation, as it is possible to distinguish the pathogen of STI from the patient's genitourinary tract in just 10% of cases.

The absence of clear diagnostic criteria and signs of the disease's characteristics complicate the patient's accounting. Symptoms of prostatitis are so non -specific that each doctor interprets it with most of the subjectivity and can associate it with a completely different pathology. Accordingly, the treatment approach also varies and often the patients strolling from one hospital cabinet to another without a positive dynamic for years. Prostatitis prevents a man who is confident in his sexual strength, closes his thoughts on a problem and brings him not so physically as psycho suffering.
What is a prostate and why is it necessary?
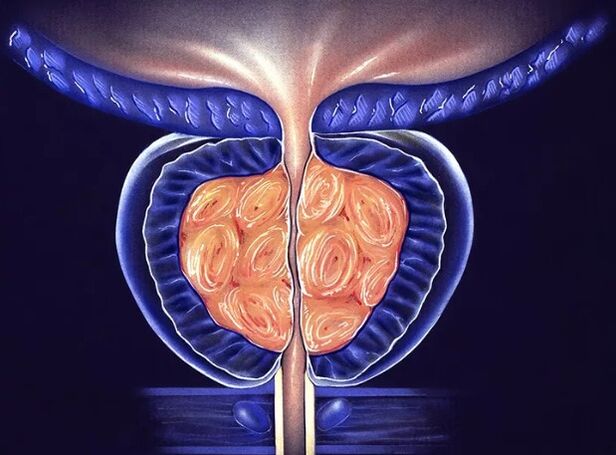
The prostate gland (prostate) is the organs of a man's small gland located around the urethra under the bladder. It is tight to beat the urethra, forming one of its sphincters - muscle jack designed to hold urine. In its shape and size, the prostate resembles chestnut beans, which is often compared to anatomy. The part of the urethra, which enters the gland is called prostatic. The back convex part of the prostate is in contact with the rectum, so it can be easily felt with the rectal finger examination. The front surface of the gland is close to the genital joints and is connected to the ligaments of the connective tissue, and the vein plexus is located between them.
The prostate gland is made up of lobules, each made by the alveoli - a small bag filled with epithelium of the secretary. The alveoli is connected to the output channel in the form of a tube, which combines with each other, enlarges and eventually falls to the medium part of the urethra. In the secretory bag, prostatic juice is synthesized and accumulated, including nutrients for spermatozoa. It allows male sex cells to maintain their activities in the female body by up to 5 days, which increases fertilization opportunities.
The gland enlightenment occurs during ejaculation. Prostatic juice is mixed with the secret of the penis and contributes 10 to 30% of the last sperm. Therefore,The prostate gland performs 2 main functions in a man's body:
- Participate in the urinary process - hold the urine when the muscle fibers are reduced and are free to pass it when they are relaxed;
- Provides sperm viability, distinguishes prostatic juice of nutrients into ejaculation.

Does the disease develop?
Prostatitis is a change in inflammation in the prostate gland and should be understood that they arise not only under the influence of bacterial microflora.The cause of inflammation can be a factor that causes damage to the gland tissue and the destruction of the cells.
Like any other tissue, the process of inflammation in the prostate continues through a certain level:
- Change - damage to prostate cells.Squirrel cytoplasms, fragments of cell nucleus, and residual membranes out of the cells that are destroyed into the intercellular space -all of which is a signal of distress for the immune system. The cells of immunity begin to actively seek to lesions, penetrate the blood vessels and connective tissue. They remove biologically active ingredients in place of damage, under the influence of blood vessels and "reinforcement" cells come.
- Exudation - the release of the blood fluid from the vessel.Under the influence of immune cells, the vessel wall extended into plasma and it rushes into the wound. If it is on the surface of the hollow organs or glands, then the blood fluid is released into the lumen, if the inflammation is tissue, then the swelling is formed. Such steps are needed to limit the focus of damage and prevent the spread of pathogens.
- Proliferation is a replacement of damaged cells with similar or connective tissue.The mechanism of germination was launched slightly earlier than the events described above and its cursing directly depends on the depth of the damage. The small focus of the destruction of the prostate gland tissue is replaced by the same functional cells and the organ restores its work completely. Disruptions are allowed through scars - replacement of dead tissue with connective tissue elements. Chronic prostatitis can eventually cause the atrophy of the prostate gland and the change in the spraying tissue to the cicatricial.
For the suggested reason, prostatitis is divided into:
- Acute bacteria- The pathogenic microflora causes serious damage to the prostate tissue with a clear inflammatory response. It often develops with infections with gonococcus and other pathogens.
- Chronic bacteria-The pathogenic bacterial bacteria or pathogenous conditions cause slow inflammation, lasting activity for more than 2 months. As a rule, pathogens are streptococci, staphylococci, E. coli, klebsiella, mycoplasma, ureaplasma, chlamydia, herpesvirus, and fungus such as candidates.
- Chronic abacteria- In the presence of inflammation in the prostate, it is not possible to detect the causal microflora. The same form of the disease develops when the urine is inserted into the prostate gland tract, the stagnation of the venous blood in the pelvis, the infringement of its emptying (rarely or excessive ejaculation). In the second case, the disease is called stagnant prostatitis.
How is the disease real?
The easiest to diagnose acute prostatitis,which continues with signs of drunkenness and clear inflammation. In a man, the temperature rose significantly to 38-39 degrees C, the pain mentioned in the perineum, in the rectum, appeared. They can give it to the thighs, in the testis, to the penis and become very unbearable until a day -to -day activity is interrupted. In some cases, the body temperature measured in the axillary cavity does not exceed the normal indicator, but the rectum in anywhere will be 1-2 degrees per normal. Signs of prostatitis are also a violation of urine: a severe urge to urinate, after which it is impossible to prevent either acute delay in the urine due to severe edema of the gland. Sometimes the drainage becomes painful, as the prostate is enlarged in the size of the rectum.
Chronic prostatitisIn its manifestation, it is so diverse that it can be easily confused with other pathologies. In the most typical case, the symptoms of prostatitis are presented:
- Pain in the throat, pelvis.It is difficult for patients to determine a particular place where it is localized, often spreading into the thighs, scrotum, head and penis firm, sacrum. The severity can be different: from almost indistinguishable with stupid or attractive. Often, pain is associated with urine or ejaculation, occurs at the end or at the beginning of the process.
- A violation of urine- Patients often urge to clear the bladder, they should be repeatedly waking up at night to urinate. However, jet pressure is normal, urinary retention rarely develops.
- Harassment- Against the background of persistent discomfort in a man's crotch, erection worsen and self -confidence is gone. The violation is worsened if pain is associated with ejaculation moment: the patient cannot fully rest, as it expects unpleasant sensations.

As a rule, with chronic prostatitis, the general well -being of a man is not interrupted, the body temperature is preserved normal throughout the disease.
How is the disease diagnosed?
Diagnosis is established by a doctor's urologist or an andrologistAfter examining the patient, collect anamnesis and study the symptoms. Doctors need to know the patient's contraception, the presence of STIs in the sexual partner, the possibility of an anal contact without a condom. This data facilitates the diagnosis and directs the doctor's thinking in the right direction. Prescription of the symptoms of the disease or discomfort in the perineum allows us to evaluate the course of prostatitis and its severity. Urologists should study the patient's genital organs and perform the rectal examination of the prostate gland. To do this, he inserted one finger into the back of the patient and grabbed the prostate that stands out on the front wall of the rectum. The pain and size indicate the intensity of the inflammatory process.

Further, doctors conducted several instrumental, microscopic, bacteriological and immunological studies to explain the cause of the disease. The most common diagnostic method is a 4 or 3-read urine sample. The first method is more time and difficult to practice in practice, as it requires patients several times to consciously disrupt urination. The second renovation is easier: the patient continues to urinate into three different containers in the same part. The first part speaks of the state of the urethra, the second about the pathology of the bladder and the kidneys, from the third, information on the condition of the prostate gland is obtained. All collected materials are studied under a microscope. With prostatitis in the third part of the urine, leukocytes and sometimes bacterial is found.
Access for prostate and massage studies while collecting secrets
For microscopy, the secret of the prostate gland is also taken.To do this, the doctor performs the prostate sequence through the rectal wall for some time so that it is emptied into the urethra. Tin is made from materials collected in the laboratory, painted and studied under high hikes. Signs of inflammation are leukocytes, bacterial etiology of disease - bacteria in smear. To determine the type of pathogen, the prostatic secret is sown in the nutrient media. If pathogenic microorganisms are present, then after 3-5 days they form a microbial colony, which can then be studied by the bacteriological method allows you to get data on microflora sensitivity to antibiotics.
Instrumental diagnostic methods , :
- Kidney ultrasound;
- Prostate beliefs with dopplerography - ultrasonic sensors are inserted into the rectum for the best visualization of the prostate gland, its blood flow is also evaluated;
- Rising ugly, needed with a stubborn course. The X -ray contract was introduced into the urethra, after which several consecutive images were made.

Starting chronic prostatitis treatment, you should adapt to a long struggle, as it is not always possible to cure it in a few weeks or even months. It is recommended to combine various methods and tools for therapy, useful for increasing drug therapy with households. With unstable prostatitis, normal sex is required, interrupted sexual action is unacceptable. Psycho -anemotional background of patients is important: depression, depression, problems in personal life and sexual field can deny all doctors' efforts.
How to prevent?
Prevention of prostatitis includes:
- The use of contraceptive barrier methods (condoms), especially when it is related to anal sex;
- Timely STI treatment;
- Normal sex life, brings relationships with full ejaculation;
- Prevention of material injuries, when class, traumatic sports should be used by all possible protection methods;
- Compliance with personal hygiene;
- Ensuring adequate physical activity.
Although today prostatitis is not associated with the risk of developing adenomas or prostate cancer, the disease brings a lot of suffering to its owners. A man who is tired of chronic pain, experienced his sexual weakness, is tired of prolonged treatment, changes that feel with an external and experienced doctor defines such a patient at first sight. To avoid such fate, you need to be careful about your health, carefully protected with each new partner and treats sexually transmitted diseases in time. Prostatitis is not fully treated in all cases, but experienced urologists can significantly improve the patient's condition and quality of life.






















